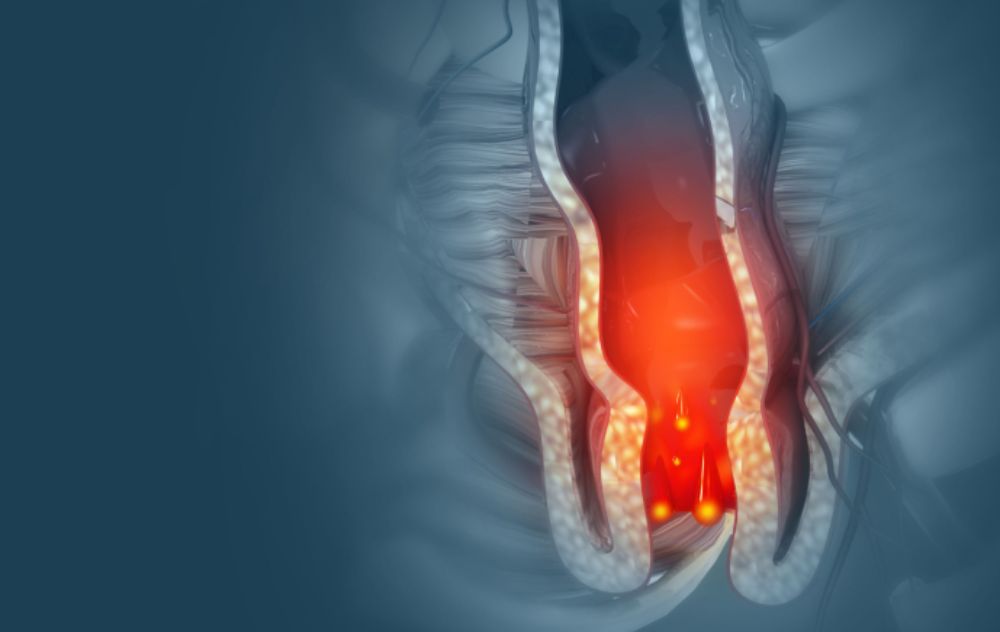
Hemorrhoids are one of the most common and uncomfortable conditions affecting adults. Symptoms like bleeding, pain, itching, swelling, and recurrent flare-ups can significantly impact daily life. Fortunately, several modern treatment options exist—including sclerotherapy and Hemorrhoid Artery Embolization (HAE).
Both treatments are minimally invasive, but they work very differently, and each may be better suited for certain types of hemorrhoids or symptom severity.
If you’re comparing these two options, this guide will help you understand how they work, their benefits, and which patients typically see the best results.
What Is Sclerotherapy for Hemorrhoid?
Sclerotherapy is a non-surgical, office-based procedure used to treat internal hemorrhoids. It is one of the earliest minimally invasive hemorrhoid treatments and continues to be widely used today.
How It Works
A physician injects a specially formulated solution (a sclerosant) into the hemorrhoid tissue. This causes the vein walls to stick together, cutting off blood flow. The hemorrhoid shrinks over time and symptoms gradually improve.
Best For:
-
Internal hemorrhoids (Grade I–II)
-
Patients with mild to moderate symptoms
-
Patients looking for a quick, in-office treatment
What Is Hemorrhoid Artery Embolization (HAE)?
Hemorrhoid Artery Embolization is an advanced, minimally invasive treatment performed by an interventional radiologist. Instead of treating the hemorrhoid itself, HAE targets the arteries supplying blood to the hemorrhoids.
How It Works
During HAE, a physician inserts a tiny catheter into an artery (typically near the groin or wrist). Using image guidance, they locate the arteries feeding the hemorrhoidal tissue and place small particles to block blood flow. Over time, the hemorrhoids shrink and symptoms improve.
Best For:
-
Chronic or recurring hemorrhoids
-
Internal hemorrhoids that cause significant bleeding
-
Patients who want to avoid surgery
-
Patients who prefer a comprehensive, long-term solution
Benefits of HAE
-
No incisions
-
No general anesthesia
-
Targets the source of hemorrhoids by reducing blood flow
-
Effective for moderate to severe internal hemorrhoids
-
Minimal downtime—most patients return to normal activity quickly
-
Lower risk of complications compared to surgery
Because HAE treats the arterial supply rather than the hemorrhoids themselves, it may offer more durable relief for patients with recurring symptoms.
Sclerotherapy vs. Hemorrhoid Artery Embolization
| Feature | Sclerotherapy | HAE |
|---|---|---|
| Best for | Mild to moderate internal hemorrhoids | Moderate to severe internal hemorrhoids |
| How it works | Injection shrinks the hemorrhoid | Blocks blood supply to hemorrhoids |
| Anesthesia | None | Local anesthesia + sedation |
| Downtime | Minimal | Minimal |
| Long-term effectiveness | May require repeat sessions | Longer-lasting relief |
| External hemorrhoids | Not effective | Not typically used |
| Treats underlying cause | Partially | Yes – targets arterial supply |
When to Seek Help
You should consider professional hemorrhoid treatment if you experience:
-
Persistent bleeding
-
Pain or swelling that interferes with daily life
-
Symptoms returning after home remedies
-
Frequent flare-ups
-
Difficulty sitting
-
Large internal hemorrhoids
Early treatment can prevent worsening symptoms and reduce your risk of complications.
Find the Right Hemorrhoid Treatment for You
Modern hemorrhoid care is more advanced, effective, and minimally invasive than ever. Whether you’re exploring sclerotherapy or HAE, the best treatment depends on your specific symptoms and goals for relief.
