
You’ve probably heard the usual advice for easing hemorrhoids, such as eating more fiber and drinking more water. Your diet can make a real difference, as it impacts your bowel habits. When certain foods contribute to constipation or diarrhea, hemorrhoid symptoms like itching, swelling, discomfort, or bleeding may flare up.
By understanding what foods trigger hemorrhoids, you take proactive steps in reducing your risk of flare-ups or alleviating symptoms.
How Certain Foods Trigger Hemorrhoids
Diet directly affects your bowel health. Low-fiber diets, in particular, slow digestion and lead to hard or infrequent stools. This causes a person to strain during a bowel movement, which places pressure on the rectal veins and contributes to the development or worsening of symptoms.
Some foods and drinks also promote hemorrhoid inflammation or irritation in certain people. Spicy foods, alcohol, and caffeine are commonly reported triggers—not because they directly cause hemorrhoids, but because they increase stool urgency, loosen stools, or contribute to dehydration. Dehydration makes stools harder and more difficult to pass, increasing strain during bowel movements and discomfort afterward.
Foods That Trigger Hemorrhoids

Foods that trigger hemorrhoids often worsen constipation, inflammation, dehydration, or rectal irritation. Common hemorrhoid trigger foods include the following:
Low-Fiber Foods
Refined grains, such as white bread, white rice, pasta, and breakfast cereals are a few examples of low-fiber foods that can cause hemorrhoid flare-ups.
Spicy Foods
Salsa, hot peppers, chili-based sauces, and red pepper flakes can irritate the rectal lining and intensify burning or itching.
Processed Foods
Fast food, packaged snacks, frozen meals, and other processed foods are typically low in fiber and high in sodium, which can increase bloating and constipation.
Caffeine
Caffeine in coffee, tea, and energy drinks can contribute to dehydration. While coffee may stimulate bowel movements, it can also increase irritation for some people.
Fried and Fatty Foods
French fries, doughnuts, bacon, cookies, and potato chips slow digestion and may worsen constipation.
Dairy Products
Cheese, milk, and ice cream can cause gas, bloating, and harder stools in some individuals.
Other Potential Trigger Foods and Drinks
- Red meat: Harder to digest and low in fiber
- Excess salt: Can contribute to swelling
- Alcohol: Causes dehydration, constipation, and blood vessel dilation
- Carbonated beverages: Increase gas and bloating
Foods That Help Prevent Hemorrhoids

Fiber plays a central role in hemorrhoid prevention by softening stools and reducing straining during bowel movements. This eases pressure on the rectal veins, helping to prevent or alleviate hemorrhoid symptoms.
Examples of high fiber foods include fruits, vegetables, whole grains, and legumes. Soluble fiber can also help regulate stool consistency.
You do not want to overdo how much fiber you eat. If your diet is low on fiber, it’s best to increase your intake in small increments over time to avoid bloating, gas, diarrhea, and constipation. The Academy of Nutrition and Dietetics suggests you should work toward 14 grams of fiber for every 1,000 calories eaten.
When a High-Fiber Diet Isn’t Enough
Some patients will still feel hemorrhoid symptoms despite adjusting their diet. Fiber may soften the stool for easier passing, but it cannot shrink internal hemorrhoids that have become chronically enlarged or prolapsed.
Internal vs External Hemorrhoids
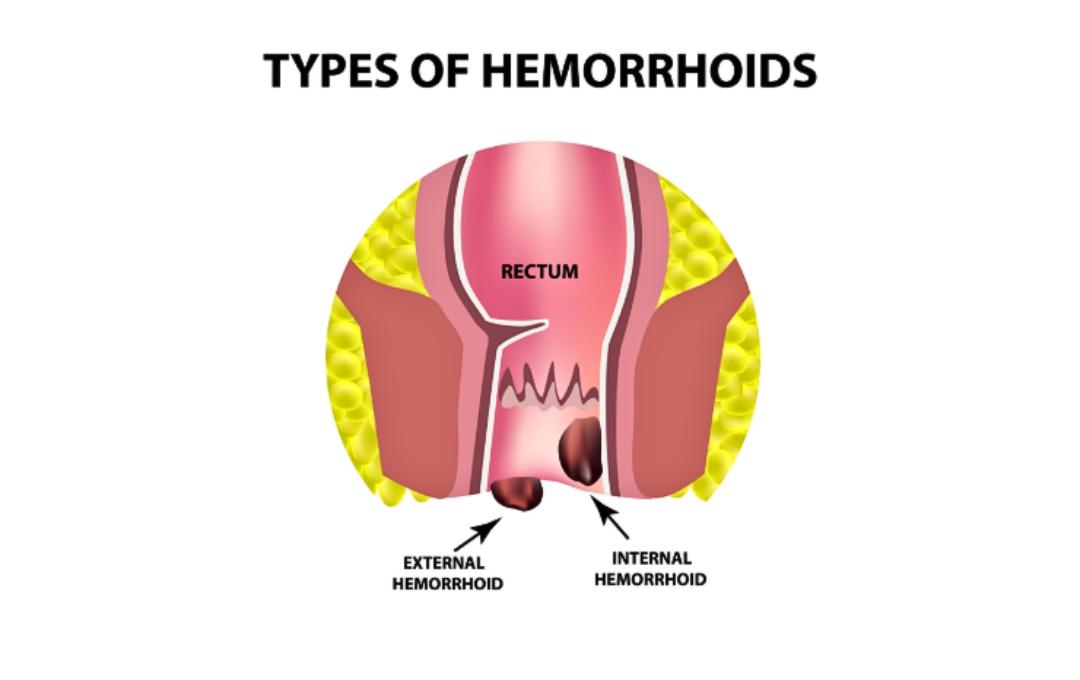
Hemorrhoids can develop either inside the anus (internal) or around the anus (external). While internal hemorrhoids are not as painful as external hemorrhoids in their early stages, they can become significantly painful when they extend outside the anus (prolapse).
When internal hemorrhoids prolapse, medical treatment may be needed to reduce the size of the prolapse and its accompanying symptoms.
How Non-Surgical Hemorrhoid Treatment Can Help
If bleeding, swelling, and itching from hemorrhoids persist after diet adjustments, hemorrhoid artery embolization (HAE) may help. This minimally invasive treatment is an outpatient procedure that’s specifically designed for internal hemorrhoids.
HAE works by reducing blood flow to the hemorrhoids, allowing the affected tissue to shrink naturally over time and alleviating bleeding and swelling. Patients do not need to plan for surgery or a hospital stay. In fact, patients can return to their daily routines shortly after treatment. Most patients experience minimal discomfort, and treatment involves only a small access site that is covered with a bandage.
Expert Internal Hemorrhoid Care at USA Hemorrhoid Centers
While diet can play an important role in managing hemorrhoid symptoms, USA Hemorrhoid Centers specializes in the advanced treatment of persistent internal hemorrhoids.
Our doctors focus on accurately diagnosing hemorrhoids to ensure hemorrhoid artery embolization (HAE) is the right path for your specific condition. Our evidence-based treatment can be personalized for each patient’s condition, helping many individuals achieve meaningful and lasting relief from hemorrhoid symptoms.
We participate in most health insurance plans, including Medicare and Medicaid, and patients can verify coverage in real time when scheduling an appointment online or by calling (855) 805-4247.
FAQs About Foods that Trigger Hemorrhoids
Foods high in fiber, such as fruits, vegetables, whole grains, and legumes, help soften stools and reduce straining.
Water is the best choice. Adequate hydration helps prevent constipation and keeps stools soft. Fiber-rich drinks like prune juice, aloe vera juice, and herbal teas may also help with hemorrhoid symptoms.
Reducing straining, managing bowel habits, and medical treatments such as HAE are the most effective ways to shrink hemorrhoids when symptoms persist.
