
Hemorrhoids are a common condition affecting millions of adults, often causing symptoms like itching, bleeding, swelling, and rectal discomfort. But some individuals also report experiencing headaches around the same time their hemorrhoid symptoms flare. This leads to an important question: Can hemorrhoids cause headaches?
The Relationship Between Hemorrhoids and Headache
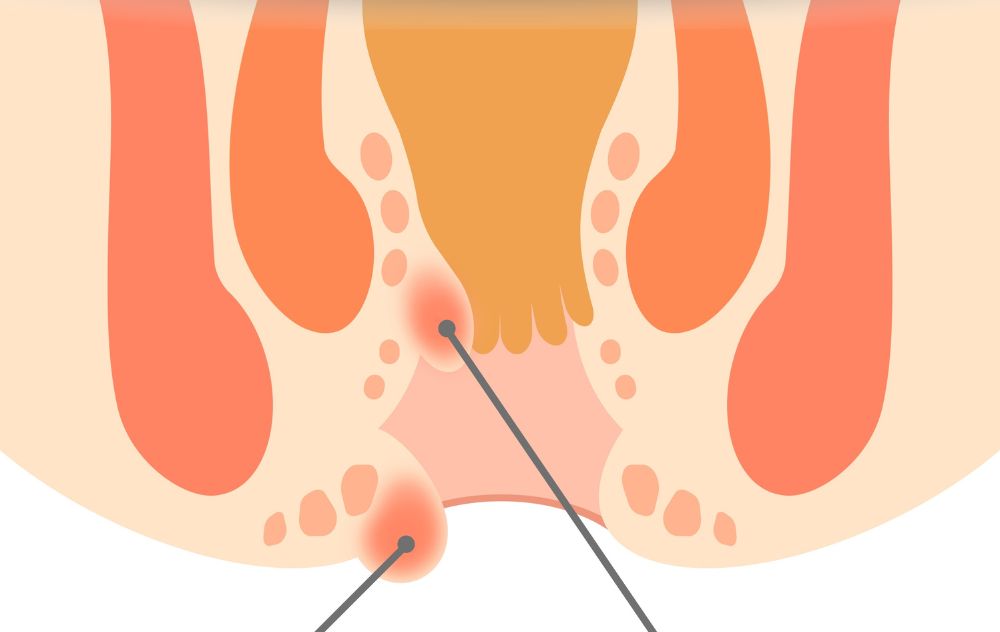
Hemorrhoids do not directly cause headaches. They are swollen veins in the rectal area, whereas headaches originate from nerves, muscles, or blood vessels in the head. However, several indirect factors related to hemorrhoids may contribute to headaches, making the connection more complex than it appears.
Here are the most likely reasons someone with hemorrhoids may also experience headaches:
-
Pain and Physical Stress
Moderate to severe hemorrhoid pain can increase stress hormones, cause muscle tension, and disrupt sleep. Chronic discomfort may lead to tension-type headaches or worsen existing migraine patterns. -
Straining During Bowel Movements
Constipation is a major risk factor for hemorrhoids. Frequent straining increases pressure in the abdomen and rectum, but it can also cause temporary spikes in blood pressure and muscle strain in the head and neck, which may trigger headaches in susceptible individuals. -
Dehydration
Many people with hemorrhoids adjust their diet, take fiber supplements, or avoid drinking enough water due to bloating or bathroom anxiety. Dehydration is a well-known trigger for headaches and migraines. -
Iron-Deficiency From Chronic Bleeding (Less Common)
In cases where hemorrhoids bleed regularly over long periods, mild iron-deficiency anemia may develop. Symptoms of anemia can include fatigue, lightheadedness, and headaches. This is not common but can occur with untreated bleeding hemorrhoids. -
Medications and Lifestyle Changes
Some over-the-counter pain relievers used for hemorrhoid discomfort—such as NSAIDs—can trigger rebound headaches when used frequently. Dietary changes, reduced caffeine intake, and poor sleep during flare-ups may also contribute.
Are Headaches a Sign of a More Serious Problem?
Headaches are not considered a primary symptom of hemorrhoids. If headaches are severe, persistent, or accompanied by neurological symptoms, rectal bleeding, weight loss, or changes in bowel habits, it is important to rule out other gastrointestinal or neurological conditions.
When to Seek Medical Evaluation
You should consider speaking with a medical professional if you experience:
• Headaches plus unexplained or heavy rectal bleeding
• Headaches that worsen with coughing, straining, or bending
• Headaches accompanied by dizziness, fatigue, or shortness of breath
• Hemorrhoid symptoms lasting longer than one week
• Hemorrhoids that cause significant pain or interfere with daily life
How to Reduce Hemorrhoid-Related Discomfort and Headaches
Because headaches in this context are usually indirect, relief comes from addressing both bowel habits and overall comfort.
Helpful strategies include:
• Increasing hydration to support digestive function
• Eating a high-fiber diet (vegetables, fruits, whole grains)
• Using stool softeners when medically appropriate
• Avoiding caffeine or alcohol excess, which can dehydrate
• Using warm sitz baths for rectal discomfort
• Managing pain appropriately with physician guidance
• Maintaining regular physical activity
• Improving sleep patterns during flare-ups
Can Treating Hemorrhoids Help Reduce Headaches?

If headaches are being triggered by pain, dehydration, or straining, then yes—treating hemorrhoids and correcting underlying bowel issues may reduce headache frequency.
However, if headaches persist even after hemorrhoid symptoms improve, it’s worth evaluating other potential triggers unrelated to digestive health.
Hemorrhoid Artery Embolization
When conservative care fails to control bleeding or discomfort, minimally invasive treatment options are available. One emerging option is Hemorrhoid Artery Embolization (HAE). During HAE, an interventional radiologist uses imaging guidance to identify and block the arteries supplying blood to internal hemorrhoids. By reducing blood flow, hemorrhoids shrink and symptoms such as bleeding and prolapse improve over time.
Unlike surgical hemorrhoidectomy, HAE does not involve removing tissue. Patients typically experience less pain, minimal downtime, and can return to normal activities faster than with traditional surgical approaches. This makes HAE an attractive option for patients with recurrent internal hemorrhoids or bleeding who are seeking non-surgical solutions.
USA Hemorrhoid Centers specializes in minimally invasive hemorrhoid treatment, including Hemorrhoid Artery Embolization. Their centers focus on resolving internal hemorrhoids at the source, helping patients reduce pain, bleeding, itching, and other disruptive symptoms. With a patient-centered approach, advanced imaging, and office-based treatment capabilities, USA Hemorrhoid Centers provides an option for individuals who want to avoid surgery while achieving lasting symptom relief.
More on Hemorrhoid Artery Embolization
Final Thoughts
So, can hemorrhoids cause headaches? Yes, they can indirectly. Hemorrhoids themselves do not create neurological or vascular changes that produce headaches. However, the pain, dehydration, stress, straining, and lifestyle adjustments associated with hemorrhoids can indirectly contribute to headaches in some individuals.
If headaches develop during hemorrhoid flare-ups, treating the underlying bowel issues and improving hydration often helps. If headaches are persistent or occur alongside significant bleeding or neurological symptoms, it is important to seek medical evaluation to rule out other causes.
