
Pregnancy causes significant physical shifts, though some are less openly discussed—such as hemorrhoids. These swollen rectal veins, which can cause pain, itching, and discomfort, are common during pregnancy. Understanding why they happen and what you can do about them is the first step toward relief.
What Are Hemorrhoids?
Hemorrhoids are swollen blood vessels in the rectal or anal area, similar to varicose veins. They can occur inside the rectum (internal hemorrhoids) or around the anus (external hemorrhoids).
Learn More About Internal vs. External Hemorrhoids
If you have hemorrhoids during pregnancy, you may notice symptoms such as:
- Itching or irritation around the anus
- Pain or discomfort, especially when sitting
- Swelling or a lump near the anus
- Bleeding during bowel movements
- A feeling of fullness in the rectal area
What Increases Hemorrhoid Risk During Pregnancy?
Pregnancy increases the risk of hemorrhoids, and existing hemorrhoids may become more painful or swollen as your body changes. Several factors work together to create added pressure in the rectal area:
Hormonal Changes
During pregnancy, higher levels of progesterone relax the smooth muscles of the digestive tract. While this helps your body adapt to pregnancy, it also slows down bowel movements. The result is constipation, which makes stools harder and more difficult to pass. Straining from constipation directly irritates rectal veins, making hemorrhoids more likely to form or worsen.
Increased Pelvic Pressure
As the uterus expands, it exerts more pressure on the veins in the lower pelvis and rectum. This added weight restricts blood flow, causing veins to swell. The further along you are in pregnancy, particularly in the third trimester, the more likely you are to feel this increased strain.
Constipation and Straining
Constipation is one of the most common triggers for hemorrhoids in pregnancy. Hard stools force you to push harder during bowel movements, which increases pressure on rectal veins. Over time, this pressure can cause the veins to bulge, resulting in painful or bleeding hemorrhoids.
Bathroom Habits
Spending too much time sitting on the toilet—whether scrolling on your phone or simply waiting—can worsen hemorrhoids. Sitting in this position puts added pressure on the rectum. Straining while on the toilet has the same effect, aggravating existing hemorrhoids and making new ones more likely to develop.
Iron Supplements
Many pregnant women are prescribed iron to support healthy blood levels, but high doses can cause or worsen constipation. This side effect makes hemorrhoids more likely to appear or become irritated. If you’re experiencing constipation from iron, ask your doctor about switching to a slow-release formula, adjusting your dosage, or adding stool-softening foods and fluids to your daily routine.
How to Prevent Hemorrhoids During Pregnancy
While you may not be able to avoid hemorrhoids completely, healthy daily habits can reduce your risk.
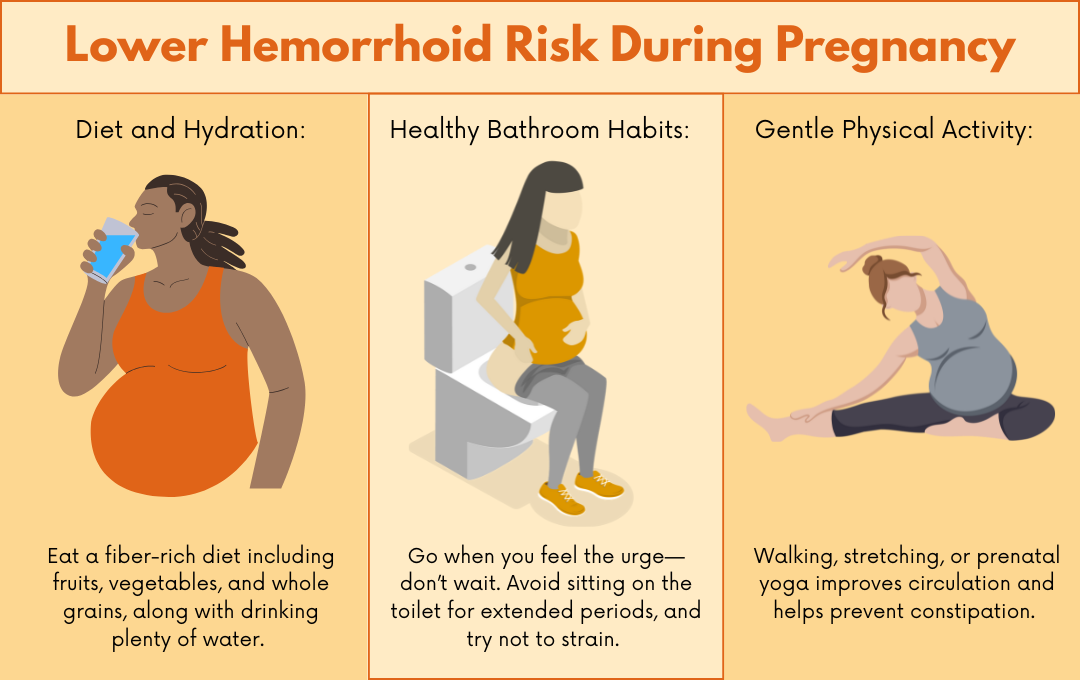
Diet and Hydration
Aim for 25–30 grams of fiber per day from foods like berries, leafy greens, lentils, and whole grains. Start your morning with oatmeal topped with fruit and include vegetables with lunch and dinner. Drink at least 8–10 glasses of water daily to keep stools soft and digestion regular. Herbal teas and water-rich foods like cucumbers or watermelon can also help with hydration.
Healthy Bathroom Habits
Respond promptly when you feel the urge to have a bowel movement to avoid constipation. Limit toilet time to no more than 5 minutes per visit and keep your feet slightly elevated on a small stool to reduce strain. Avoid reading or scrolling on your phone in the bathroom, as this increases rectal pressure.
Gentle Physical Activity
Engage in 20–30 minutes of light movement most days of the week, such as walking after meals, prenatal yoga, or stretching exercises. Activities like pelvic tilts and gentle squats can also improve circulation and support bowel function. Always consult with your healthcare provider before beginning or adjusting your exercise routine.
Safe Management of Hemorrhoids During Pregnancy
If hemorrhoids do appear, several safe options can ease symptoms.
At-Home Relief
- Warm sitz baths to soothe irritation
- Cold compresses to reduce swelling
- Witch hazel pads or unscented wipes for gentle cleaning
- Donut cushions to relieve pressure while sitting
Medications With Doctor Approval
- Acetaminophen (Tylenol) may be safe for pain relief.
- Certain topical creams or suppositories may be prescribed, but only use under medical guidance.
What to Avoid
Skip strong steroid creams, oral hemorrhoid medications, or surgical procedures during pregnancy unless specifically recommended by a physician.
Do Hemorrhoids Go Away After Pregnancy?
In many cases, hemorrhoids shrink or disappear within a few weeks postpartum, especially with proper hydration, diet, and bowel habits. However, severe hemorrhoids or persistent constipation may cause them to linger. If symptoms continue, medical evaluation is important.
When to See a Doctor for Hemorrhoid Symptoms

Consult a healthcare provider if you experience:
- Persistent or heavy bleeding
- Severe pain that doesn’t improve
- Signs of infection or clotting
- Ongoing hemorrhoids despite home care
If your symptoms do not resolve after delivery, treatment may be necessary.
Minimally Invasive Hemorrhoid Relief After Pregnancy
For women whose hemorrhoids persist after childbirth, hemorrhoid artery embolization (HAE) is a safe, nonsurgical treatment available at USA Hemorrhoid Centers.
- What it is: A minimally invasive, image-guided procedure that blocks blood flow to hemorrhoids, helping them shrink.
- Benefits: Outpatient care, quick recovery, and less invasive than surgery.
- Who may benefit: Those with severe or recurring hemorrhoids that do not respond to conservative care.
USA Hemorrhoid Centers specialize in this advanced treatment, helping patients find relief without the downtime of surgery.
Frequently Asked Questions About Hemorrhoids and Pregnancy
Hemorrhoids are very common during pregnancy, especially in the third trimester. Increased pelvic pressure and hormonal changes put pregnant women at higher risk.
No. While uncomfortable for you, hemorrhoids do not affect your baby’s health.
At home remedies like sitz baths, witch hazel pads, and doctor-approved topical treatments can provide relief for hemorrhoids during pregnancy. Always consult your provider before using medications.
If hemorrhoid symptoms like pain or bleeding become severe or if hemorrhoids don’t improve with self-care during pregnancy, seek medical attention.
Yes, hemorrhoids can return with subsequent pregnancies, but preventive steps like diet, hydration, and exercise can help.
